Written by Bria Fredericks. Reviewed by Diana Licalzi, MS, RD, CDE
An Overview of the Insulin Response
Insulin resistance is the underlying cause of type 2 diabetes, but what exactly results in insulin resistance? This blog will dive deeper into the biochemistry of how and why individuals develop insulin resistance and what precisely that means for their health going forward. Before jumping into how insulin resistance develops, it’s crucial to understand how insulin works in a healthy, non-diabetic individual:
- After we eat a meal, our digestive system breaks down the carbohydrates into smaller sugars, namely glucose, which can then transport into the bloodstream.
- As glucose enters our bloodstream, the pancreas receives a signal to release a hormone called insulin.
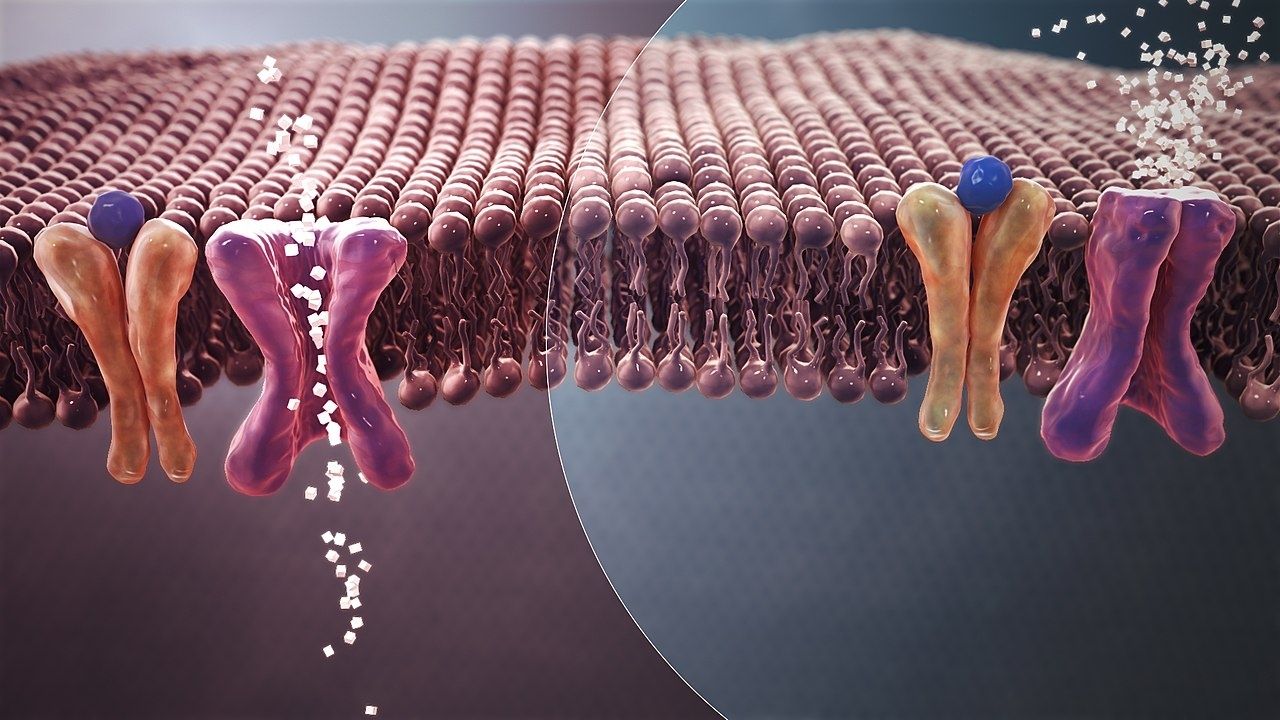
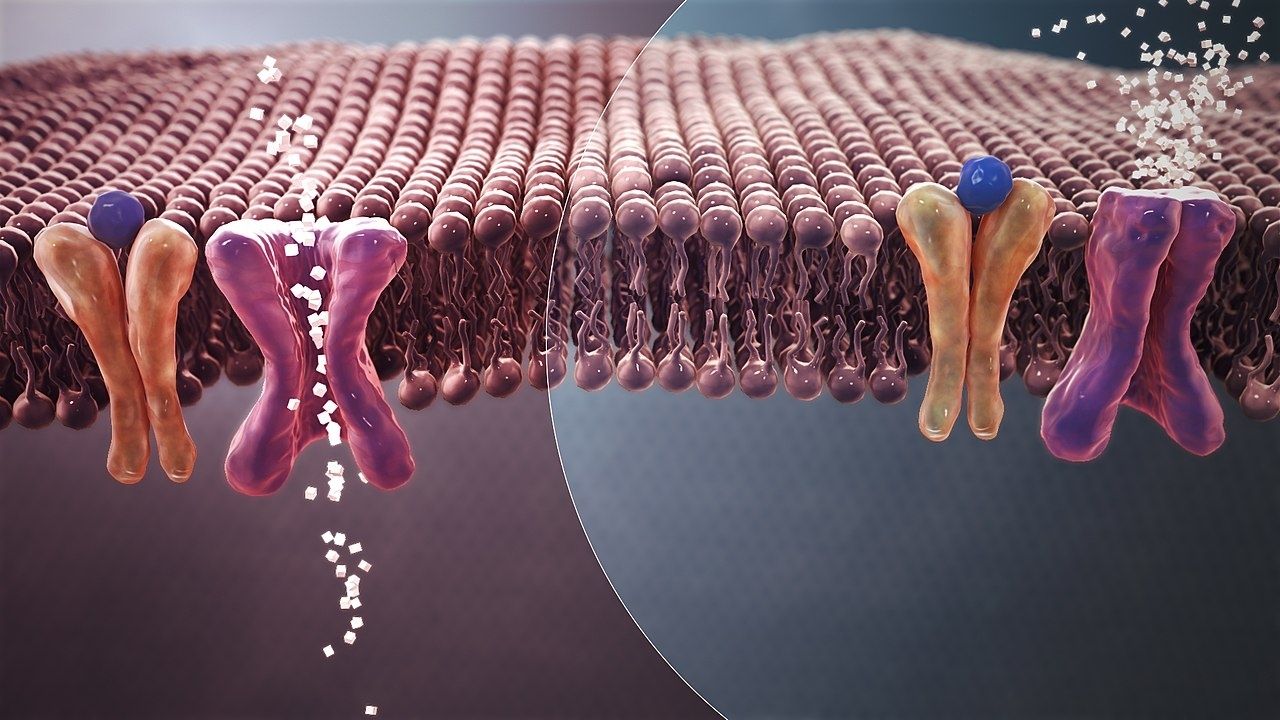
- Insulin then travels to muscle and fat cells and binds to receptors on the cell membranes, indicating glucose in the blood (see Figure b below).
- The binding of insulin to these receptors sends a signal that causes GLUT4, transport proteins, to travel to the cell membrane (Figure b).
- Once at the cell membrane, the GLUT4 transporters allow glucose to enter the cell from the blood (Figure b). As glucose enters the cells, blood glucose levels drop back down to a normal range.
- Cells then either store the glucose or use it to make energy, depending on what they need at that time.
- Insulin’s primary role is to maintain blood sugar homeostasis, or balance, within your body and the bloodstream.

In people with type 2 diabetes, glucose cannot enter the cells, leading to a buildup of glucose in the blood. This results in hyperglycemia, or high blood sugar. Over time, this causes damage to the pancreas because it must continuously pump out insulin as it attempts to control the high glucose levels. Blood vessels also begin to harden over time due to chronically elevated glucose levels, leading to cardiovascular disease.
Why Does Insulin Resistance Develop?
There are a few explanations as to why insulin resistance develops, but the exact cellular mechanisms are still being researched. Recent research demonstrates that insulin resistance develops from a continuous energy surplus in the body. Evolutionarily, our bodies were not programmed to waste energy so any food we consume is either used right away or stored as fat for later use.
Unfortunately, though, our bodies contain a finite number of adipose (fat) cells, and there is a limit as to how much fat they can hold. Thus, as our cells store more and more fat, they reach capacity, causing them to swell and trigger an inflammatory response. This response downregulates, or shuts off, the insulin receptors on the cell membrane. As more insulin receptors shut off, less GLUT4 transporter molecules are activated. As previously mentioned, the activation of GLUT4 transporters allows glucose to leave the blood and enter the cell. Therefore, the result of this inflammatory response leaves an individual with high blood sugar.
Who’s To Blame: Carbohydrates or Fat?
People often blame insulin resistance on carbohydrate intake, but, as noted above, research shows that the problem stems from the use and storage of fat. An increase in fat leads to the overfilling of adipose (fat) tissue, causing the problematic inflammatory response. This 2002 study demonstrates the exact mechanism—when cellular fat levels rise, it inhibits the insulin response, leading to a decrease in GLUT4 transporters at the membrane, ultimately leaving glucose trapped in the blood.
In addition, other studies have specifically examined the relationship between diets high in animal, saturated fat compared to plant-based, unsaturated fat. For example, in this 2016 study, Koska and colleagues demonstrated a correlation between insulin resistance and high saturated fat diets. Koska found that a saturated fat diet induced insulin resistance in both healthy and glucose-tolerance-impaired individuals. As you can see from the graph below, plasma glucose (blood sugar) levels were much higher in people on a high saturated fat diet than on a standard, healthy diet.

To further expand on this point, another study, conducted by Azemati and colleagues in 2017, found that (1) increased animal protein intake correlated with insulin resistance, and (2) with increased plant protein intake, insulin resistance did not change. Figure 4 shows how insulin resistance skyrocketed in participants who consumed more and more animal protein (like red meat), but showed no worsening of insulin resistance in participants who consumed plant proteins (like legumes, for example).
Can Insulin Resistance Be Reversed?
Numerous studies show that a plant-based diet is the most effective way to control insulin resistance. In 2009, Barnard and his team demonstrated that a plant-based diet could both manage and reverse insulin resistance. In this study, participants with type 2 diabetes were asked to consume either a conventional diet or a vegan, plant-based diet. After a few weeks, the participants on the vegan diet showed significant decreases in their HbA1C levels. Interestingly, participants in both groups lost weight, but only participants in the vegan group showed improved hbA1C levels.

Studies also demonstrate that exercise can alleviate insulin resistance. Exercise increases the expression of GLUT4 and increases the number of activated GLUT4 transporters that travel to the cell membrane. This leads to more glucose flowing into the cell and out of the blood (Richter, Hargreaves, 2013). To read more about the incredible relationship between exercise and type diabetes, read this blog.
To Recap What We Know about Insulin Resistance
- Type 2 diabetes develops from insulin resistance.
- The insulin response relies on transporter molecules, called GLUT4, to bring glucose from the blood and into the cell.
- Excess fat produces an inflammatory response that disrupts the insulin pathway.
- High-fat diets (especially when the fat is from animal products) correlate with high insulin resistance.
- Plant-based diets, along with exercise, are the most successful way to increase insulin sensitivity and reverse insulin resistance.
References:
Fat vs. Sugar in the War on Insulin Resistance, That Sugar Movement. (2020). Retrieved 15 September 2020.
Glucose Regulation. (2020). Retrieved 15 September 2020.
Harrar, S. (2020). Insulin Resistance Causes and Symptoms. Retrieved 15 September 2020, from https://www.endocrineweb.com/conditions/type-2-diabetes/insulin-resistance-causes-symptoms
Kojta, I., Chacińska, M., & Błachnio-Zabielska, A. (2020). Obesity, Bioactive Lipids, and Adipose Tissue Inflammation in Insulin Resistance. Nutrients, 12(5), 1305. https://pubmed.ncbi.nlm.nih.gov/32375231/
Richter EA, Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev. 2013; 93:993-1017.
https://pubmed.ncbi.nlm.nih.gov/23899560/
Sears, B., & Perry, M. (2015). The role of fatty acids in insulin resistance. Lipids Health Dis., 14(121). (2020). Retrieved 15 September 2020.
Diana is a nationally recognized Registered Dietitian and Certified Diabetes Care and Education Specialist (CDCES), and holds a Master’s degree in Nutrition Science and Policy from the Tufts Friedman School of Nutrition. She received her education and dietetics training from Villanova University, Tufts University, and UC San Diego Health. Diana has over 8 years of experience working in the field of type 2 diabetes.


Leave a Comment